Medical Business. Simplified.
One Fully
Integrated System.
Everything Flows. Everything is Verified.
For Speedier Payments with Minimal Rework.
Data Management/Acquisition
Electronic Information and Documentation Acquisition, secure, and efficient data acquisition for patient analysis.

Charge Management
The most critical step in the financial success of billing services and medical practices.

Claims Management
Improve your claims processing and reduce cycle time, leading to increased efficiencies, time and money savings, and faster reimbursements.

Denial Management
Easily access documents, appeal templates, and key denial metrics for insight into root causes for denials allowing
quick remedial action.


Insurance Payment Processing
Automates the insurance payment process, identifies under payments quickly and minimizes filing risks for improved efficiencies.

Insurance Follow-up
Automated payer/plan solutions give you status of any claim in the adjudication process.

Patient Engagement
Real-time reports, integrated pass-through to the health records portal, options for preferred method of communication optimize the patient experience.

Reporting
Delivers automatic and ad-hoc reports on virtually every aspect of your practice, staff performance, and claims inventory/reimbursement.

Data Management/Acquisition
Capturing patient and billing data and documentation typically includes manual entry, often leading to human error. PHIMED technology leverages OCR and electronic data field mapping for accurate, secure, and efficient data acquisition. PhyGeneSys has the extra quality control step in validating the accuracy of information recorded at this stage to prevent inaccurate data from creating more issues downstream.
There are numerous benefits of automated and validated; here are three:
1) Reducing manual entry through automation helps eliminate human error, reduces staff time and practice administrative costs, and allows your practice to scale up without additional staff.
2) Data aggregation contributes to more complete billing by aggregating more comprehensive records. Data from multiple sources is harmonized data for transparent analysis in the treatment process.
3) While exceptionally valuable in assuring quicker claims reimbursement, data management also empowers opportunities for continuous process improvement through KPIs and actionable intelligence. You’ll be able to quickly identify areas of your workflow, staffing, and practice procedures that fall below expectations and set a corrective course of action.

Charge Management
Capturing all charges is perhaps the most critical step in the financial success of medical practices, surgery centers, and other health systems. An effective charge capture process reduces claims denial and revenue mistakes, increasing error-free submissions.
Effective charge management begins by establishing internal and third-party Codes and Service Descriptors, ideally ones that are easily understood by providers, payers, and patients.
Secondly, internal codes need to match external codes for accurate integration. Failing to match providers, referring providers and insurance plan code sets to internal charge codes leads to missed payment for services rendered.
Finally, your process must have checkpoints for capturing/entering every service your team provides. PHIMED will work closely with your team to ensure no code is overlooked. For example, PhyGeneSys automatically posts electronic transactions into the system; the process is faster, more accurate, and frees up staff to work in other areas.


Claims Management
Improve your claims processing and reduce cycle time, leading to increased efficiencies, time and money savings, and faster reimbursements. In addition, improve financial performance with automated, clean, and data-driven medical claims management.
The PhyGeneSys system is designed to automatically verify that every claim is clean and error-free before submission. In addition to streamlining the claims management process, PhyGeneSys‘ validated accuracy eliminates the costly, time-consuming rework typically associated with rejected or underpaid claims.
Claims management software allows providers to review codes and services and verify that each claim is properly coded and contains the correct information before the claim is submitted for reimbursement.
Our goal is to reduce claim denials, corrections, and rebilling and improve first-time pass-through rates for optimal reimbursement using real-time claim edits, real-time eligibility and electronic claims attachments.

Denial Management
Scrubbing data early in the claims process helps resolve the issues leading to non-approved medical claims and mitigate future denial risk, reducing rework and ensuring faster payment. PhyGeneSys provides a proven workflow, easy access to source documents, appeal templates, and key denial inventory reporting metrics, and permits streamlined denial intervention for rapid revenue recovery. In addition, you will gain insight into root causes for denials allowing quick remedial action. As you receive this feedback, you can expect to reduce future denials and rejections by improving claim accuracy and increasing efficiency and staff performance with automation.
It’s easy for staff to check the claim and appeal status, document all interactions with the insurance company, patient, or responsible party and produce appeal documentation. As a result, you can minimize denial write-offs and improve your bottom line by providing your coding staff with a denial management system.


Insurance Payment Processing
Through best-in-class automation and data verification, PhyGeneSys makes insurance payment processing a seamless task. PhyGeneSys automates the insurance payment process, identifies underpayments quickly, and minimizes filing risks for improved efficiencies. Process every contract and know exactly what you’re supposed to get paid and when you’re not getting paid appropriately.
With PhyGeneSys, you can fully automate the insurance payment process for improved efficiencies. You have all the data and information to check the claim status and make informed decisions to minimize filing risk. Ensure you’re being paid appropriately and create work queues to follow up on if not. Again, it’s very important to identify underpayments and resolve them quickly.

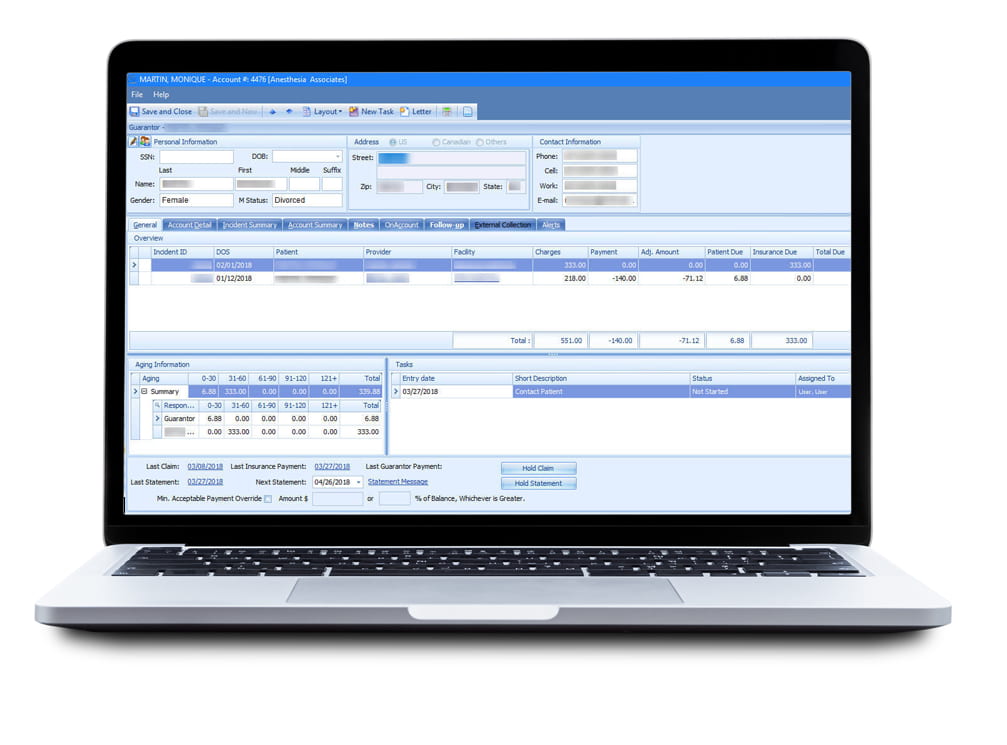
Insurance Follow-up
Automated payer/plan solutions give you the status of any claim that has not been adjudicated. You won’t achieve maximum revenue if you don’t follow up on denials. Even if you meet timely filing standards for the initial submission of a claim, you will also be on the clock when reworking and appealing denials.
Know your denial codes: insurance payers issue claim denials using remittance advice codes that include brief explanations. Review these codes to determine whether to correct and resubmit the claim or bill the patient. And remember, there are many reasons a claim may be denied. For example, Workers’ Compensation may deny payment until attachments are sent. The electronic claims attachments substantially reduce denials. Payers may withhold payment due to a lack of medical necessity or because services took place outside of the appropriate time frame.


Patient Engagement
Effective and timely communication regarding account balances has become a key factor in maximizing patient payments. PhyGeneSys allows the patient to select their preference form of communication (paper, electronic statements, email and/or text). All communications in all forms are integrated into the system and are accessible by the patient and the providers’ staff. Copies of communications are maintained electronically in the system and in the patient portal.
Improving patient engagement can also lower healthcare costs. The technology in place to help your patient engage in your practice is the best way to increase patient satisfaction and grow your practice. PHIMED can assist you and your team with improved patient engagement through our integrated software system, regardless or your specialty or business model.

Reporting
Our automated technology delivers a vast range of standard and customized reports, including valuable exception reporting that identifies areas requiring attention using predictive data. Robust reporting is the cornerstone for operational efficiency. The PhyGeneSys system delivers automatic and ad-hoc reports on virtually every aspect of your practice and claims reimbursement. You’ll know the productivity ratio of your team, payer trending analysis and a root cause analysis, Claim Inventory and A/R Reports, and many others.
Accurate, timely reporting and analytics is a strong data foundation that can help you:
- Improve administrative efficiency and quality of care
- Display KPIs for easy interpretation
- Measure financial performance, manage cost and improve revenue
- Mitigate the risk of revenue loss